D1 Hockey Player with Hip Labral Tear and Sports Hernia: Evaluation Insights
Dr. Mike and Dr. Colin got together recently to talk about how they would assess an athlete with a hip labral tear and sports hernia.
You can check out the whole conversation on YouTube!
This was inspired by an introduction to a D1 college hockey player who had played through a hip labral tear for an entire season last year: then discovered he ALSO had a sports hernia!
Despite the name, a sports hernia isn’t like a traditional hernia, where your abdominal contents behind your core muscles bulge out of a tear in your abs. There is no bulge or tear in the abdominal wall with a sports hernia. It’s a label for chronic groin/lower ab pain, often in athletes, and is frequently missed or misdiagnosed.
If you want the deep dive into sports hernias, check out this article by Hopkins et al.
Back to our case!
Our college hockey player started having hip pain and groin/lower stomach pain in the middle of his season.
He managed to play through it - but realized that something was wrong because it never completely went away and caused him issues with his day to day life.
He got an MRI towards the end of the season and found out that he had a hip labrum tear in his left hip, and a sports hernia.
Click here to hear Dr. Mike talk about what a labral tear is on an Instagram reel.
His surgeon didn’t recommend that he needed surgery - so he decided to try to recover with physical therapy.
When we talked with him last week, he was mostly pain free with everyday activities, and could exercise and train mostly without pain. He knew he wasn’t completely through with his recovery though - he would get abdominal and hip soreness on his left side with sprinting, and any “triple extension” movements. Check out the picture below for an example of what triple extension looks like.
Image of triple extension. Credit: https://talktomejohnnie.com/hip-extension/
He was already doing physical therapy with another PT clinic when we first talked with him.
He has 5-6 more weeks of summer until he’s back to school and wanted to get a second opinion on what he could do to be ready to return to hockey at full performance and without pain.
Here’s what we knew we wanted to assess during his initial evaluation after meeting this athlete, and what we found during that eval:
Hip range of motion
Sports hernias are also found with losses of hip range of motion, and with higher rates in the presence of other hip injuries like femoroacetabular impingement (Hopkins et al 2017).
His previous physical therapy was heavily focused on strengthening the muscles around his hip.
We want to make sure his hip can comfortably move on its own, and actively, in as many directions as possible.
We found that our hockey player was lacking some mobility in pretty much every single direction in his left hip. Most notably, he was missing some hip internal rotation and hip extension compared to his non-symptomatic side. He had hip discomfort with bringing his left hip towards his chest, and turning his hip towards the middle of his body.
We immediately began improving his symptoms and hip range of motion with some exercises to get his abdominals to tolerate getting longer and improving his ability to move into hip extension without his lower back arching.
What does his running and sprinting look like?
We always watch our patients perform tasks that cause them symptoms (as long as we decide it's safe to do that).
Due to injury - your body can change how it used to move to help protect the injured area.
These changes, however, can shift where your body is distributing the stresses/forces of movements, and create adaptations that may not be helpful.
Our patient had significant abdominal discomfort after sprinting. We wanted to see if there was anything happening when he sprinted that might increase discomfort on his sports hernia.
We found that this patient had a tougher time getting his left foot underneath his body while running (which likely explains his lack of hip internal rotation mobility). He also showed increased side bending of his torso (see the picture below) when he was pushing into the ground on his left side compared to his right.
This is a left sidebend of the torso. Credit: https://lh6.googleusercontent.com/proxy/a_U1lFdyJh-1Tk1ZqppRps9A-WGZYD56skm_Fht_Rj3jhku7RwuzqdszvIZlT9soVuiZ04oSzDmQTwhVsenXCLboM53TfK1HQjI.
Was this from his loss of range of motion on his left hip? Was this something his body had done to protect his left hip?
We’re not going to know exactly WHY this happened - but we can relate what we see to where the stress of moving is applied in his body.
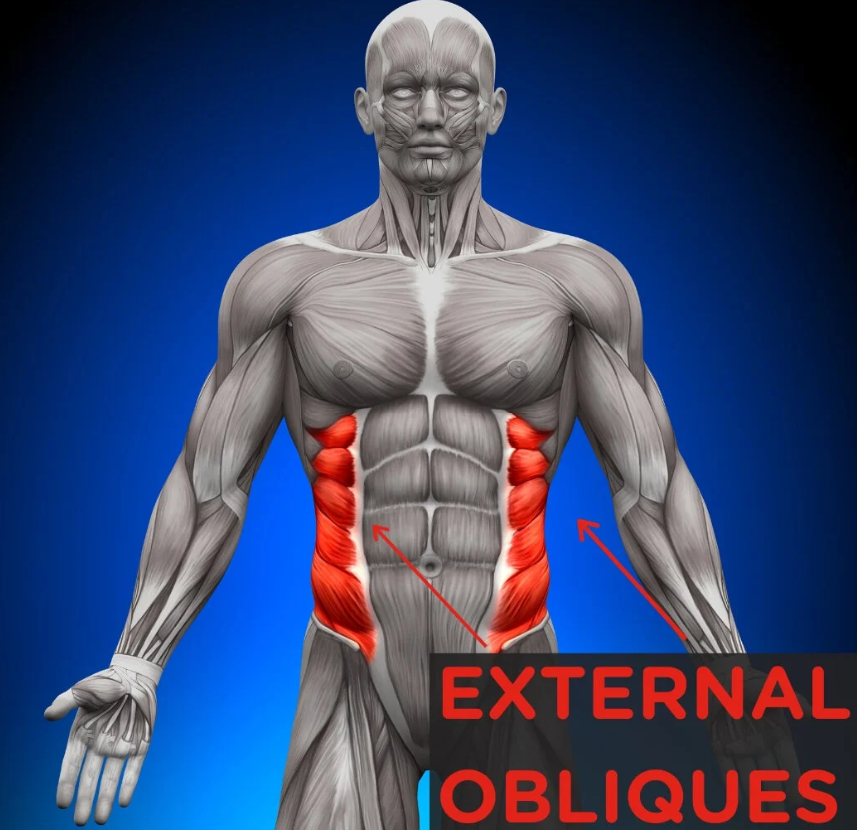
In this case: this side bending of the spine is made possible by contracting a muscle called your external abdominal oblique.
Part of the attachment of this muscle is onto the area of the groin where our patient was having symptoms after sprinting.
This side bend increases muscle tension and stress around his painful area - and COULD be a part of why his groin was still bothering him even though he was strengthening the muscles around his hip.
If we do end up continuing to work with this athlete, we would want to monitor a few things to track his progress and make adjustments to his plan as necessary:
When we regain full range of motion in his left hip, is he able to get his left foot more underneath his body while running?
If he is able to get his left foot more underneath him, does this change the degree of sidebend in his torso?
Most importantly: If we are able to create some positive changes in his running technique, what happens to his symptoms? Do they get better? Do they get worse? Or do they stay the same?
We hope this inside view of the Vital PT thought process during a specific examination was helpful!
We want every potential patient to know exactly what to expect when they choose to work with us: a thorough evaluation to identify the root cause(s) of your pain.
We regularly work with patients who have been frustrated by doing other physical therapy without getting the results they wanted.
This series is to start to show how we may do things differently than someone's past provider and what makes Vital PT special.
Stay tuned for more posts about examinations, treatment sessions, plans of care and different diagnoses!
Interested in learning more? The best way to do that is by booking a free 20-minute phone call with me.
During this call, we can talk about anything you want! Whether it’s about a current injury or pain you’re dealing with, how to improve your current programming, or if you just want to chat with me more about Physical Therapy, I’m always happy to help!